Breast Cancer
Questions and Answers
Q1. What is Breast Cancer and how does it begin?
A. Like the skin, the lining of the mouth, and other organs, the glands in the breast are in a constant state of reproduction. This constant renewal is stimulated throughout a woman’s lifetime by the primary female hormone, estrogen. To ensure perfect reproduction, any imperfect or “bad” cells that are produced during this process typically die or are destroyed by the body’s defense systems.
Sometimes, however, an imperfect cell remains unchecked by the body’s defenses. If it begins to reproduce, it can develop into a cancerous tumor that, as it grows, may invade the local breast tissue as cancer. If left untreated, some of these tumor cells can break off and travel to other parts of the body.
Q2. How does a woman get breast cancer?
A. The short answer is we just don’t know. Extensive research has been conducted on diet, exercise, local environmental factors, family history and other possible causes contributing to breast cancer in an effort to determine what causes cancers to grow. However, with the exception of estrogen (female hormone) stimulation and strong family history (genetic causes) in some patients, the reasons why some women develop breast cancer while others do not remain a mystery. The fact is, for most women, cancer “just happens,” and they do not have an identifiable risk factor.
Q3. Can I prevent breast cancer?
A. Prevention works for some cancers. For example, cigarette smoking can cause cancers of the mouth, swallowing tube, lungs, bladder, etc. Consequently, not smoking is one of the best cancer-prevention measures. For some women who have already had one breast cancer or whose family history or genetics place them at high risk, certain medicines have been shown to prevent or delay breast cancer. For most women, however, there is no effective breast cancer prevention strategy. Instead, the best way to “prevent” cancer is to find it early. Of course, for women with a strong family history of breast cancer, close monitoring is essential as these women have an increased risk of developing breast cancer.
Q4. Will early detection help me?
A. Yes. The earlier the cancer is found, the more likely the cure. In fact, patients who find cancer at the earliest stages have a more than 90 percent chance of long-term cure.
Q5. What are the best methods of early detection?
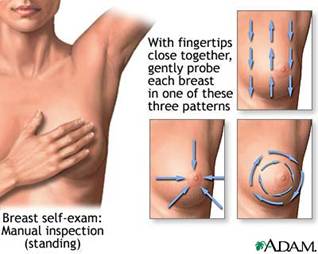
A. The best methods for finding breast cancer are monthly self-exams conducted by you or your partner, annual physical examinations with your doctor and, beginning at age 35 - 40, annual x-rays of the breasts known as mammograms. This combined approach is known as “breast cancer screening.”
Q6. What is a mammogram? I’ve heard they were painful.
A. A mammogram is a special type of x-ray used to create detailed pictures of the breast. The x-ray dose is very low, and the system is designed specifically for imaging the breasts. This simple x-ray does require pressure on the breast, which may cause discomfort for several seconds. However, this "annual discomfort" could save your life. Because screening mammography can detect 85 percent of breast cancers, including tumors too tiny to be felt, this non-invasive procedure is one of the best tests for early detection. However, because 10 to 15 percent of breast cancers do not show up on a mammogram, regular self-exams and physician visits are still important.

Q7. What happens if the doctor finds a suspicious area?
A. If something suspicious is found, you may be referred for additional tests including close-up x-rays and/or ultrasound (sonography). A breast biopsy also may be recommended. Thanks to new advances in biopsy techniques, for most women, the biopsy is a relatively painless outpatient procedure done with a needle under local anesthesia. Samples of the breast tissue are taken and examined under a microscope for cancer cells. In most instances — 80 percent of the time — breast biopsies indicate that the breast lumps are benign tumors or other non-cancerous masses. These lumps could be the result of connective tissue, fibrocystic growths or scar tissue from past injuries. These growths are called “benign tumors” because they do not spread to other organs and are not life threatening. In the other 20 percent of cases, if the biopsy confirms cancer, or if cells are suspicious for cancer, the cancer in the breast will need treatment.

Q8. What are the steps in curing breast cancer?
A. We know that if a woman’s cancer is cured locally in the breast and systemically in other parts of the body, then she is cured. So, curing breast cancer requires: 1) local cure of the cancer in the breast and 2) systemic cure — the control or prevention of cancer cells that have or might have spread to other parts of the body. Surgery and radiation therapy are used to control the cancer locally, and chemotherapy is used to treat microscopic cells that may have traveled to other parts of the body. The ultimate goal is to cure the cancer in the breast itself and keep the cancer from coming back elsewhere.
Q9. How rapidly does breast cancer spread?
A. The rate at which breast cancer spreads is different for each woman but usually takes years to develop. Like many other cancers, breast cancer usually follows an orderly progression from a pre-invasive state, which we call ductal carcinoma in-situ, or DCIS, to invasive ductal carcinoma.
As DCIS progresses, it can break through the wall of the duct into the fatty tissue of the breast, and invade the surrounding normal breast tissue, resulting in infiltrating (or invasive) ductal carcinoma (IDC). When it infiltrates the lobules of the breast, the cancer is called infiltrating (or invasive) lobular carcinoma (ILC). Both IDC and ILC types of cancer are treated by either mastectomy or BCT.

Q10. Are there different types of breast cancer?
A. Yes, because the cancer changes as it develops. DCIS or “In-situ cancer” means the tumor is confined to the area where it began, so DCIS refers to cancer that still is contained only in ducts and has not yet invaded the tissues of the breast or spread to other parts of the body. (The figure above is an illustration of in-situ cancer growing in the duct, but not invading the breast tissue.) More than 95 percent of women diagnosed at this early stage can be cured so, again, early detection translates into early cure.
Q11. How does a doctor determine how much cancer I have?
A. Following a breast cancer diagnosis, the cancerous lump needs to be removed, and in most cases, the lymph glands under the arm are removed and tested for cancer spread. Frequently, additional tests to look for cancer in other parts of the body, like bone scans, x-rays or CT scans may be ordered as well. The results of these diagnostic procedures are used to stage the cancer.
Q12. What do you mean by staging and why is that done?

A. Doctors estimate how much cancer a woman has with an internationally recognized staging system for breast cancer. By staging the cancer they can determine which local treatments a woman may have and how likely it is that the cancer may have spread to other parts of the body. The staging system assigns a number for: tumor size, T, nodal status, that is, whether it has spread into the nodes, N, and the presence or absence of metastasis, M. These stages help doctors compare treatment results among similar patient groups. They also provide women and their doctors with information needed to assess treatment.
Q13. Do the staging numbers impact a woman’s chance of cure?
A. In general, the less cancer a woman has, the lower the TNM numbers. Lower stage means a greater chance of long-term cure. Recent findings from the National Cancer Institute suggest that five-year survival rates are greater than 95 percent for confined, low-stage cancers (Stage 0, 1 and some Stage 2 cancers), 75 percent for cancers that have spread to the surrounding tissue (Stage 2 and 3 cancers), and 20 percent for cancers that have metastasized (Stage 4 cancers).
B. TREATMENT OPTIONS
Q14. After a breast cancer diagnosis, what proven local treatment options are available for women?
A. Depending on several factors including access to health care, tumor and breast size,heredity factors and immune disease, a woman may have the choice of:
Mastectomy is the removal of the entire breast. Mastectomy is the oldest method of modern breast cancer treatment and can control the cancer on the chest wall. However, mastectomy results in loss of the normal breast contour and normal breast and nipple sensation.
Mastectomy with Reconstruction is for women who want to retain a normal breast contour, but whose tumors are too large to remove without significantly distorting the breast. Mastectomy with reconstruction restores the normal breast contour. However, normal breast and nipple sensations are lost because the majority of tissue is removed.


Breast Conservation Therapy (BCT) — Lumpectomy followed by Breast Irradiation, is shown above. In BCT, the surgeon removes tumor growth and the rim of tissue around the tumor. The tissue is then analyzed to make sure all the cancer cells are gone. Several weeks later, or following chemotherapy if prescribed, radiation therapy (irradiation) is delivered to the breast to destroy any remaining cancer cells that may have moved undetected beyond the surgical field. When properly performed, BCT preserves the normal breast contour and normal sensation of the skin and the nipple.
Q15. Has Breast Conservation always been an option for treating breast cancer?
A. No. Breast conservation therapy is a major, modern advance in the treatment of women with breast cancer. In the early 1900s, Dr. William Halstead developed the concept of Radical Mastectomy, an operation that made it possible to gain both local control and cure of breast cancer for some women. The radical mastectomy was, however, an extensive procedure, requiring the removal of the muscles of the chest wall as well as the entire breast.
By the mid-1960s, medical doctors began to understand that they might be able to achieve both local control and cure of breast cancer without a radical mastectomy. They conducted trials to see if a lesser form of surgery, known as Total Mastectomy, could cure cancer in the breast as well as radical mastectomy. Total mastectomy was different in that, while the entire breast was still removed, the chest wall muscles underlying the breast remained intact. Research showed that this less drastic treatment offered women a better functional result without compromising local control and cure of cancer.
However, despite these results and the improved quality of life that total mastectomy offered over radical mastectomy, it took some surgeons many years to accept that the radical mastectomy was no longer necessary. Even in the 1970s and 1980s, women were still being treated routinely with radical mastectomy for breast cancer. While most doctors keep up with proven advances in treatment, a few could not shake the notion that “more is better.”
Q16. Then how was breast conservation tested for safety and effectiveness?
A. National organizations in the United States and other countries took the concept of limited breast surgery one step further. They performed randomized trials comparing three treatment options:
- Total mastectomy, which had already proven equivalent to radical mastectomy.
- Lumpectomy (in which only the breast tumor was removed).
- Lumpectomy followed by radiation therapy to the breast
The results of these trials showed that, regardless of whether the patient was treated with total mastectomy or lumpectomy and radiation (appropriate BCT), breast cure rates and survival were virtually identical. With either of these approaches, the local recurrence rate was only about 10 percent at 10 years. However, for patients who had lumpectomy only with no follow up radiation, the cancer came back in the breast 40% of the time.
Q17. Does this mean that removing the breast doesn't mean better cure?
A. For women with early stage breast cancer--and that is most women diagnosed today--that is exactly right.. Many worldwide medical trials involving thousands of women showed that mastectomy does not improve cure rates for women with early stage cancer. In fact, in 1990, the National Institutes of Health Consensus Statement on Breast Conservation indicated that “The preferred mode of treatment for women with early stage breast cancer is lumpectomy followed by breast irradiation”, otherwise known as appropriate BCT.
Q18. Is appropriate Breast Conservation Therapy in wide use now?
A. When the National Institute for Health (NIH) Consensus Statement, which recommended appropriate BCT for Stage I and Stage II breast cancer, was issued 10 years ago, it was thought within several years, 80 -90 percent of eligible women would have appropriate BCT as their primary means of cancer control. But even today, in more than half of the cases, available data indicate that doctors still treat their patients with either mastectomy or lumpectomy alone. Only about 60 percent of women with Stage 1 breast cancer and 35 percent of women with Stage 2 cancer actually receive appropriate BCT, lumpectomy followed by radiation treatment. These figures have remained stable for the last several years.
Q 19.Why didn’t the endorsement of the NIH result in widespread adoption of lumpectomy followed by radiotherapy for early stage breast cancer?
A. Despite overwhelming evidence clearly documenting equivalent results of breast conservation therapy and mastectomy, some doctors simply prefer mastectomy for their patients. Mastectomy is not a "wrong" treatment for any patient, but it is a major operation which can affect a woman's appearance and quality of life without any benefit in local control or survival.
Two particularly interesting studies addressed this issue. In Colorado, older physicians were found to have a significantly higher rate of mastectomy use than more recently trained doctors. And at Baylor University, which has a radiotherapy center in its hospital, only 15% of eligible women had BCT—all the others underwent mastectomy.
In addition, some patient surveys show that women can be greatly influenced by the information that they get from their doctors. Despite published results, doctors who prefer mastectomy may inappropriately influence their patients to choose more aggressive surgery even when conservative surgery is the treatment of choice.
Q20. The National Institutes of Health termed lumpectomy followed by radiation as “appropriate BCT” and lumpectomy alone as “inappropriate BCT”. Why isn’t taking the lump out sufficient to make it appropriate treatment? Just how important is the radiation afterwards?
A. Even when physicians believe they have removed all the cancer during lumpectomy, microscopic cells can remain in the breast, even when it is thought that the cancer has been completely removed. This may be true even for small tumors.
With lumpectomy only, and no radiation therapy, cancer recurs in the breast in up to 40 percent of women. By any definition, that is inappropriate BCT. Put another way, a woman who has lumpectomy alone has four times the risk of recurrence in the breast than a woman who receives follow-up radiation therapy. This means adding radiation follow-up to lumpectomy reduces a woman’s chance of local recurrence by 75 percent.
Q21. I think I am a candidate for BCT. But I am convinced that my doctor seems more comfortable with mastectomy than breast conservation. I would like a second opinion. How do I get one?
A. Simply make an appointment with another physician that is recommended by friends and/or health care resources. Or come meet with any of the physicians at ROA. We will review all of your options with you objectively and thoroughly. We can show you the facts and figures on the various treatments you are considering.
Q22.My doctor removed an invasive cancer from my breast but said it was small enough that I wouldn’t need to have followup radiation. Based on what you’ve told me, I’m concerned that’s not right. Can you advise me?
A. Several groups across the country have examined all types of invasive breast cancers and their recurrence rates following lumpectomy only. One of the most recent trials examined women with tumors 1 centimeter or smaller whom they also felt would benefit from hormone therapy. The trial compared tamoxifen (a female hormone blocker) only, radiation only, or radiation and tamoxifen.
Even in this highly selected, very favorable group of patients, women who received radiation had one-third the recurrences of women who received hormonal therapy only, and women who received hormones and radiation had one-fifth the recurrence rate. Their results clearly demonstrate that women who wish to preserve their breast should have followup radiation therapy.
Q23. Is there a time when breast conservation may not be the best treatment?
A. Yes. There are a few circumstances in which Breast Conservation Therapy may not be the recommended treatment. These include:
- If the breast cancer is multi-centric — for example, if the cancer is present in more than one area of the breast or if all the cancer cannot be removed with a single incision.
- If a woman’s cancer is more than 2 inches in size — most radiation oncologists and surgeons agree that a tumor size greater than 5 cm (2 inches) is too large for breast conservation because of a higher risk of local recurrence. On the other hand, women with larger tumors and/or 4 or more positive lymph glands have been shown to benefit from post-mastectomy radiation. So radiation therapy remains an important treatment in this case, even if the breast cannot be preserved. Occasionally, however, pre-operative chemotherapy can make some women eligible for Breast Conserving Therapy, if the tumor shrinks enough.
- If, after a second attempt at removing the lump there are still extensive positive margins (all of the cancer cannot be removed), there is a much higher likelihood of local recurrence.
- If the tumor is large in proportion to the breast. In this case, too much breast tissue would have to be removed with poor cosmetic results.
- If a woman has certain connective tissue diseases, like scleroderma.
- If a woman has genetic predisposition to breast cancer.
Q24. I was told I have Ductal Carcinoma In-Site (DCIS). How do I know if I am a candidate for lumpectomy followed by radiation therapy?
A. In most cases, a woman is a candidate for breast conservation if she has a non-invasive tumor (DCIS) or an early cancer (T1 or T2) that can be removed safely while leaving adequate tissue for a good cosmetic result
Q25. I have a very small amount of DCIS. My doctor says that with this small amount, I will not need radiation. What do you think?
A. First, as we have read, DCIS is different from invasive cancer. Treatment of very small DCIS lesions of 5 millimeters or less is a highly controversial area, and some doctors have begun to advocate treating highly selected patients with lumpectomy only. While we do not want to disagree with your doctor’s recommendations, we will say that there is no long-term data from any national trial to support this approach. Recent summaries of trials conducted here and in Europe continue to show a three times higher recurrence rate for women who undergo lumpectomy only, regardless of the size of the tumor.
Rather than simply not be treated, we believe that women who have a small DCIS lesion should consider enrolling in a clinical trial such as RTOG 98-04. This trial compares lumpectomy only to lumpectomy and radiotherapy. That way, regardless of your outcome, other women can benefit in the future from your decision.
You are welcome to call us if you wish to consider enrolling in a clinical trial.
Q25a. If I had a mastectomy, might I still benefit from radiation therapy?
A. For some women who have mastectomy, radiation therapy is a very important part of treatment. National experts agree that post-mastectomy radiation therapy is necessary if the tumor is more than 5 cm (2 inches) in size, four or more lymph glands are involved, or if there are positive margins (cut-through tumor). Radiation therapy can also help some women who may not meet these absolute criteria but have other findings placing them at higher risk for local recurrence.
Q25b. How does the addition of radiation therapy help in such a case?
A. Women with large tumor size and/or multiple positive lymph nodes are considered to be at high risk for local and regional recurrence of breast cancer, as high as 40%. The addition of radiation dramatically improves a woman’s odds of remaining cancer-free.
Additionally, important trials also demonstrate a significant improvement in survival for women who receive post-mastectomy radiation therapy. If you have had a mastectomy, we encourage you to call ROA for an independent opinion as to whether you may benefit from the addition of radiation therapy.
C. RADIATION THERAPY
Q26. What exactly is radiation therapy, and how is it performed?
A. Radiation therapy is a very specialized form of X-ray treatment. Precise, high energy x-rays deliver cancer killing radiation where it is needed while protecting other parts of the body. When carefully delivered, radiation therapy kills microscopic tumor cells that remain in the breast, while preserving normal breast tissues. When a woman has radiation treatment, nothing touches her — it’s similar to getting a chest x-ray, except that the radiation is given expressly to the breast.
Treatments usually take a few minutes per day over a six or seven week period. Patients will meet daily with the therapists who deliver your radiation treatments. Your physicians meet with you at least weekly and more frequently as needed.
Q27. A friend of mine said that if she had breast cancer she would just remove the whole breast because she’s afraid of radiation treatment. Is radiation something to fear?
A. No. Radiation therapy is one of the most effective means of cancer control and cure ever developed. Correctly administered, radiation therapy is able to stop cancer in its tracks while preserving healthy, normal areas. As we stated earlier, using radiation treatment with lumpectomy improves the chance of curing the cancer in the breast by 75 percent. This allows a woman to have the same cancer cure rate in the breast as with a mastectomy.
Q28. What are the main complications I can expect from having a lumpectomy followed by radiation treatment?
A. Radiation Oncology of Atlanta has among the most experienced treatment team and the most advanced treatment machines available, so there is a very low likelihood of any kind of major complication. The most common side effect of the radiation treatment is tanning. This causes fair-skinned women to get a little pink. Dark-skinned women as well as those who tan easily find that the breast will become darker. However, rarely will the breast peel and the tanning usually resolves in several months. Women with large breasts might experience irritation under the breast. Some women can be fatigued during treatment. Like the tanning, these side effects usually resolve themselves shortly following treatment.
Q29. Can adding radiation therapy help keep the cancer from coming back in other places in the body? And if so, can it help my chances for survival?
A. For certain women the answer is yes. Several studies show that at least for women with larger tumors and/or significant lymph node involvement, the addition of radiation therapy not only reduces the likelihood of the cancer coming back in the breast or chest wall (in the case of mastectomy), but also makes it less likely that the cancer will spread to other parts of the body. A recent overview of major breast cancer trials documents an improvement in overall survival just because of the addition of radiation therapy.
Q30. I’ve recently heard about IMRT for breast cancer treatment, as well as Deep Inspiration Breath Hold. Does that make a difference?
A. Intensity Modulated Radiation Therapy
(IMRT) or electronic compensation (EC) are the newest and sometimes the
best ways to take into account all the different contours of a woman’s
body. These approaches allow the radiation oncologist and his team to
create a customized plan for each woman, minimizing the chance of hot
or cold spots. Using IMRT/EC, the patient is treated with many small
radiation beams, each of which can deliver its own specifically
designed intensity. By cross-firing the breast with these beams, our
physicians can deliver a uniform radiation dose to the tumor, while
protecting sensitive surrounding tissue from unnecessary treatment. We
believe these approaches offer certain advantages in the treatment of
breast cancer, including more sparing of critical normal tissues as
well a superior ability to conform the dose to the contour of the
breast compared with other techniques.
Deep Inspiration Breath Hold, or DIBH, is a technique for left sided
breast tumors that allows the chest and breast to be lifted away from
the heart. Through monitoring the position of the chest wall with a
technique called "VisionRT", the treatment is only given while the
chest is raised up and away from the heart. This spares the heart from
radiation therapy.
Q31. Tell me more about IMRT and the Breast Cancer Team.
A. Dr. Williams and Radiation Oncology of Atlanta’s Breast Cancer Team have had advanced training in the use of IMRT for breast cancer. The were among the first providers of IMRT technology to women in Georgia.
Q32. What about the “super-local” radiation devices I’ve read about?

A. Several manufacturers have brought to market devices that may be able to eliminate external radiation after lumpectomy. These devices deliver “super-local” radiation to the lumpectomy cavity only using temporary implants. Such a procedure of delivering radiation to a very localized area using implanted radiation sources is called "brachytherapy". Brachy means short, and therapy means treatment. In selected patients. breast brachytherapy appears to achieve the same chance of long-term control and cure as external beam radiation, but in a much shorter period of time. These techniques are generally known as "Accelerated Partial Breast Irradiation", or APBI.
Balloon brachytherapy for APBI uses a balloon catheter placed in the cavity where the tumor was removed. Balloon brachytherapy is the most extensively tested breast brachytherapy technique and shows promising results,
How is Balloon Brachytherapy performed?
Following lumpectomy, if review of the tumor shows it to be favorable for APBI, the cavity is evaluated, including its shape and the skin thickness. If these tests show the cavity to be acceptable, the treatment balloon. A CT scan is performed for treatment planning and the Physics team performs calculations to assure the dose is correct.
Over the next 5 days treatment is delivered twice a day, usually around 8:00 am and 2:00 pm. A CT is performed prior to each treatment to be sure the balloon is still in good position. Each treatment takes about 45 minutes total, including scanning and waiting for the room. Following the last treatment, the balloon is removed, post treatment instructions given and the patient is discharged with an appointment to return in a week.
For selected women with favorable breast cancers,
APBI brachytherapy appears to have a good place in treatment. The
entire treatment is given in 5 days instead of six and a half weeks. It
is convenient, easy, and seems to have good results in selected
patients. Possible late effects or complications incude fat necrosis,
persistent seroma and infection.
Women need to know, however, that while promising and
probably equivalent to standard radiation in selected cases, the
results of national randomized clinical trials are not yet available.
D. CHEMOTHERAPY
Q33. How does chemotherapy differ from radiation and surgery?
A. Radiation and surgery are local treatments that treat the breast itself. They are designed to keep the cancer from coming back in the breast. Without local control, complete cure is impossible.
Chemotherapy is different. Instead of treating locally only, chemotherapy is given in a vein and travels throughout the body to treat cancer cells that may have spread beyond the breast. So, chemotherapy is systemic treatment while radiation and surgery are local treatments. Both local and systemic control are necessary for cure of breast cancer. Chemotherapy is given by Medical Oncologists.
Common chemotherapy medicines include Adriamycin, Cytoxan and Taxol, as well as pills such as the hormone blockers, Tamoxifen, Raloxifine and Anastrazole. A new medication, Herceptin, has shown great promise in the treatment of certain breast cancer patients.

Q34. Why would I have both radiation and chemotherapy?
A. Chemotherapy helps to reduce the relative risk of recurrence and death from breast cancer by killing cancer cells that may have spread to other parts of the body. Risk reduction is a complicated idea--but put simply--suppose a woman had a 15 percent chance of recurrence or death, If she receives chemotherapy, her risk of recurrence is reduced by 1/3. So taking the chemotherapy has lowered her risk from 15 percent to about 10 percent. ( 15% minus 1/3 (5 percent) =10%) Therefore, while chemotherapy cannot guarantee a cure, it does reduce the chance that the cancer will return.
If chemotherapy is recommended, it is important to follow the medical oncologist's orders. Typically, pre-menopausal women with tumors 1 cm or larger in size (T1c or greater) are advised to take chemotherapy as part of treatment. Also, some post- menopausal women may benefit from chemotherapy based on the particular nature of their tumor. A few weeks after chemotherapy, you will receive radiation to the breast as part of the breast conserving therapy. Sometimes chemotherapy is given before surgery.
Q35. Are hormones, like Estrogen blockers, helpful?

A. In most cases, breast cancer in women, like prostate cancer in men, is hormonally responsive. This means that breast cancer cells may be stimulated to grow by estrogen, a woman’s natural hormone . Certain medications including Tamoxifen (Nolvadex) and newer drugs like Raloxifine, Arimidex and others, may act as “estrogen blockers”, blocking the effects of estrogen on cancer cells. For many women, estrogen blockers are an important part of cancer treatment. While they can be associated with some additional symptoms such as hot flashes, their overall value is undisputed.
Q36. I'm afraid of chemotherapy. Do I have to take it?
A. No one is going to twist your arm. However, medical oncologists' recommendations, whether for chemotherapy, hormonal therapy or biological therapy, are backed by research on thousands of women like yourself. The advice you receive is worthwhile, and the medications may add years of improved quality of life and survival.
There is no denying that the cancer treatment process can be confusing, frightening and frankly overwhelming . But you must remember it is better to ask questions and consider getting a second opinion rather than refuse or delay important therapy.
E. BREAST CANCER RESEARCH
Q37. You talk quite a bit about the importance of cancer treatment results. Don’t all doctors get the same results?

A. Because patients are seen by so many different specialists, is very difficult for any individual physician to track of all their patients. This is why we emphasize the importance of physician participation in clinical trials. The specific requirements of the clinical trials makes doctors, whether surgeons, medical oncologists or radiation oncologists, be aware of and follow the most current thinking in the field.
It is likely that if your physicians participate in clinical trials they will be up-to-date with the latest techniques and advances. So, in many physicians' opinion, it is both the doctor's reputation-- and participation in clinical trials--- that are your best guarantees to good treatment.
Q37. What research have you done on breast cancer?
Dr. Hamilton Williams and associates examined outcomes in several areas of interest to doctors and patients. These include:
- Overall cancer freedom;
- Cancer freedom for African American women compared to white women;
- Likelihood of local recurrence for young women;
- Whether women with small tumors need to have an axillary dissection (lymph node sampling);
- The impact of screening mammography on stage at presentation for Breast Conservation Therapy
Q39. Have you presented your data?
A. Yes. Our doctors analyzed and presented their follow-up results--included as part of a larger group--at several national and international meetings, including the American Society for Clinical Oncology, the American Society for Therapeutic Radiology and Oncology and at the prestigious European Conference on Strategies and Outcomes in Cancer among others. This study represented the largest series of patients reported in the literature from any community center in the United States. At the 10-year follow-up mark, 92 percent of patients were free from local recurrence.
And, our recent study on African-American women and breast cancer received a Blue Ribbon Award from the Georgia Cancer Coalition for “outstanding achievement in cancer research and treatment.”
Q40. How do these results compare with national figures?
A. These results indicate that women treated by our physicians with breast conservation therapy enjoy the same if not better, breast cancer cure rates as women treated in any of the major clinical trials. We found that at 10-year followup, more than 90% of these patients were able to retain their breasts. These results compare very favorably to other national and international series of women treated for breast cancer.
Q41. Does BCT work as well for black women as white women?

A. Yes. Our research, presented at several national meetings, shows that black women enjoy the same local control rate and breast preservation rate as white women. In fact, there is no difference at all.
This is an important finding because Black women and men sometimes have more aggressive cancers than their white counterparts, and there had been little information available on the effectiveness of BCT in black women.
Q41a. What is a randomized trial?
A. A randomized trial is a study by physicians of various treatment options. Physicians try to determine if a new treatment method or drug works better than the standard therapy. Patients are randomly assigned to the different treatments and their results are collected and analyzed. Many times the new treatments prove superior to traditional methods and they then become the new standard.
A woman’s participation in a trial may not only help her, but the knowledge gained may also help other women with cancer in the future. There are many national study groups and, if interested, we can help you find one that may fit you.
Q42. You have treated so many patients over the years—what do you see as the major improvements which will come to women with breast cancer in the future?
A. In all areas of cancer treatment we hope to improve survival while further minimizing the impact of treatment on quality of life. Breast conservation is one of the cornerstones of quality of life preserving treatment. It is hoped that some of the "super local" radiation therapy approaches outlined above will reduce the time it takes to deliver the radiation therapy necessary to preserve the breast. Also, for women with large breasts, "prone breast treatment" can allow better coverage of the breast tissue with fewer side effects from radiation. APBI, especially for women with large breasts and small, favorable tumors, is believed to give as high a cure rate as standard radiation with fewer side effects. IMRT and electronic compensation, covered above, allow more homogeneous treatment of the breast, again allowing an improvement in therapy with a lessened impact on quality of life.
A new approach to shortened breast cancer treatment times is "accelerated hypofractionated radiation therapy", pioneered by the Canadian and British cancer agencies. This approach, for selected women, allows the entire treatment time to be completed in 16 to 21 daily treatments, compared with the traditional standard of 33 treatments. It is not only more convenient but equally effective. It is not for every woman, though, as the greater daily dose may increase the risk of thickening or fibrosis in women with very generous breasts.Medical Oncology has made significant advances in recent years, "Dose-dense" chemotherapy can shorten the time under treatment while improving outcomes, and hormone blockers like Femara and Arimidex offer improvements over traditional hormonal therapies for post-menopausal women. Biological agents are continuing to show advances--new agents like Herceptin have demonstrated major improvements in survival for women with certain kinds of cancers.Some of the most exciting new changes in medical oncology include biologic drugs like Herceptin, Kadcyla and Perjeta, which target cell recptors for patients with HER-2 positive cancers. These new agents have made a tremendous difference in the control and cure of breast cancer.
F. FINANCIAL CONCERNS AND SUPPORT
Q43. I was diagnosed with invasive breast cancer and have been advised of my treatment options. I would like to preserve my breast, but am concerned that this will be more expensive than just having the breast removed. For me, cost is an issue. Is breast conservation more expensive?
A. Researchers have found that the cost of breast-conserving treatment is actually less than the cost of a mastectomy. This is because many of the women who had mastectomy go on to have reconstruction surgery, adding greatly to the cost of the mastectomy itself. Lumpectomy followed by radiation still appears to be a less expensive choice than mastectomy in the long run.
Q44. Will my insurance company pay for a lumpectomy followed by radiation treatment?
A. Yes, they will. This is a standard treatment for women with breast cancer and all major insurance companies.
Q45. Do you offer any support programs?
A. Yes. For breast cancer patients, programs of diet and nutritional improvement, exercise and support are increasingly important in regaining control of one's life. To that end, our affiliated hospitals offer our breast cancer patients a series of opportunities designed to improve both their mental and physical well-being as well as to develop the skills and understanding needed for a better quality of life.
Please call Radiation Oncology of Atlanta at 404-705-9192, or contact us here if you have questions or want to schedule a consultation or follow-up appointment.



